What is Achalasia?
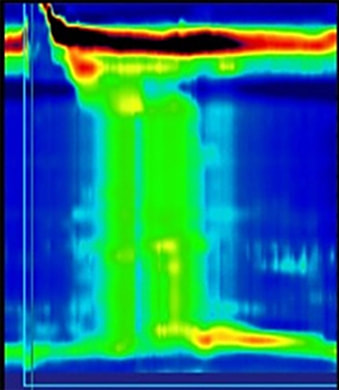
Achalasia is a rare condition that affects the nerves that supply the esophagus (inhibitory motor neurons) which results in loss of the normal contractions of the esophageal muscles. This causes impaired food/liquid propulsion and patients can experience "food sticking", regurgitation, chest pain, weight loss and heartburn. Symptoms may wax and wane but generally progress over time. With longstanding disease, the esophagus becomes dilated and tortuous and unable to pass contents into the stomach. Rarely, achalasia has been associated with development of esophageal cancer. The x-rays with swallowed contrast demonstrate an esophagus with advanced achalasia (left) and a normal esophagus (right).
How is achalasia treated?
Traditionally, achalasia has been treated by laparoscopic Hellers myotomy, pneumatic dilation, and botulinum (Botox) injection. In the recent years, a new procedure, Peroral Endoscopic Myotomy (POEM) has been introduced, and offers faster recovery after the procedure, the ability to better tailor the procedure to the patient, and is potentially more effective in patients with advanced disease.
How is Achalasia Diagnosed?
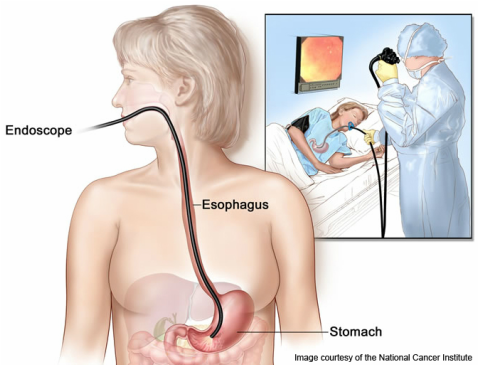
Achalasia is diagnosed using a combination of examinations that may include an endoscopy, contrast esophogram, and esophageal manometry
An endoscopy allows for the examination of upper GI tract with small flexible camera. For more information, please see this video from American Society of Gastrointestinal Endoscopy.
A contrast esophogram is taken while swallowing a liquid that can be seen on X-ray. Patients with achalasia typically have an abnormal appearance of the esophagus as a result of its abnormal contractions
With esophageal manometry, pressure readings from the esophagus are obtained using a small catheter with pressure sensors that allow the pressure and pattern of contraction along the length of your esophagus to be recorded. This information can then be used to diagnose and categorize the type of achalasia or other motility disorder of the esophagus.